Inflammation Deflation: Can Acupuncture Really Help?
Understanding Acupuncture's Role in Fighting Inflammation
Acupuncture for inflammation has gained serious attention from researchers and patients alike as a natural way to calm the body's inflammatory response. Here's what you need to know:
Quick Overview:
What it is: Fine needles placed at specific points to reduce inflammatory markers like TNF-α, IL-6, and IL-1β
How it works: Activates the vagus nerve and releases anti-inflammatory chemicals through your body's own systems
Evidence: Studies show 50% of patients report significant pain improvement, with some conditions showing 70-80% survival improvement in severe inflammation
Best for: Arthritis, IBD, asthma, chronic pain, and other inflammatory conditions
Timeline: Benefits often seen within 2-6 sessions over several weeks
When inflammation gets out of control, it can turn from your body's helpful healing response into a destructive force. Chronic inflammation links to everything from joint pain and digestive issues to heart disease and diabetes.
Traditional medications like NSAIDs work, but they come with side effects - especially for your gut. That's where acupuncture steps in as a gentler option that works with your body's natural systems.
Recent research shows acupuncture doesn't just mask symptoms. It actually changes how your immune system behaves at the cellular level. Scientists have mapped exactly how needles trigger anti-inflammatory pathways through your nervous system.
I'm Dr. Michelle Andrews D.C., founder of ChiroHer in Oklahoma City, and I've seen how combining acupuncture with chiropractic care can transform how patients manage inflammation and pain. While my primary focus is spinal health, I regularly refer patients for acupuncture for inflammation when they need that extra layer of natural healing support.
Why Inflammation Matters in Health and Disease
Imagine your body as a house with the world's most sophisticated security system. When something goes wrong - whether it's a cut on your finger or a virus trying to invade - your inflammatory response kicks in like an emergency response team rushing to the scene.
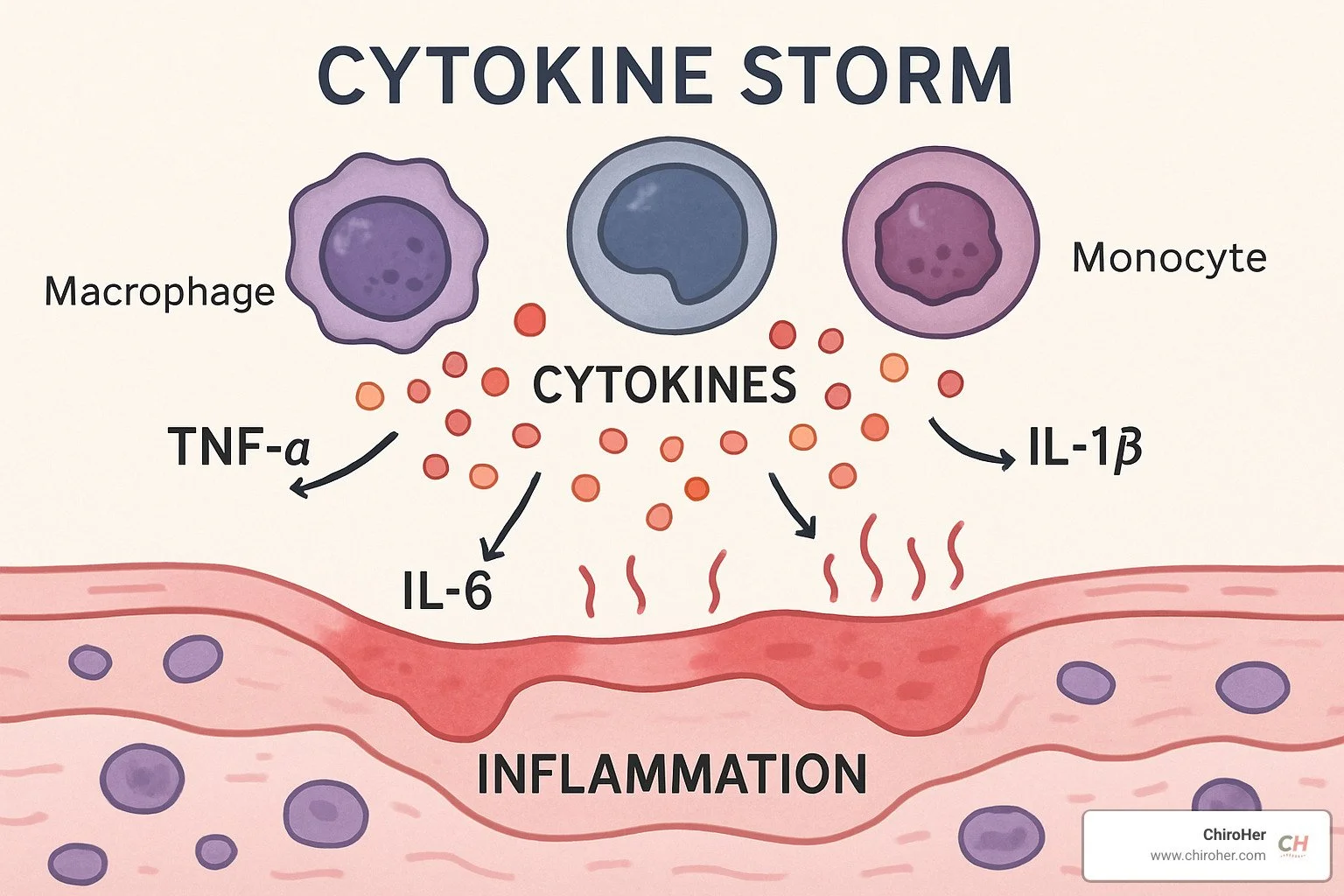
This response involves chemical messengers called cytokines that coordinate your body's defense. The main players include TNF-α (tumor necrosis factor-alpha), which sounds the initial alarm, and IL-6 (interleukin-6), which helps orchestrate the inflammatory response. There's also IL-1β (interleukin-1 beta), which contributes to the pain and swelling you feel, and NF-κB (nuclear factor kappa B), which acts like the master control switch turning inflammatory genes on and off.
When this system works as designed, it's absolutely brilliant. Your body fights off threats, heals injuries, and then everything returns to normal. The challenge comes when your internal security system forgets to stand down.
This is where acupuncture for inflammation becomes particularly valuable - it helps restore the natural balance between your body's inflammatory and anti-inflammatory responses.
Silent Fire: Chronic Low-Grade Inflammation
Chronic inflammation is like having a smoke detector that won't stop beeping. Instead of the helpful acute response that heals and protects, you get a persistent, low-level inflammatory state that slowly damages healthy tissue.
This "silent fire" creates serious health problems over time. Metabolic syndrome develops when inflammatory chemicals interfere with how your body processes sugar and fat. Your cardiovascular system suffers as inflammation damages blood vessel walls, increasing your risk of heart disease. Type 2 diabetes often follows, since inflammatory markers make it harder for insulin to do its job properly.
The triggers for this chronic inflammation are everywhere in modern life. Processed foods, chronic stress, poor sleep, and sitting too much all fan these inflammatory flames.
When the Heat Helps: Acute Protective Response
Not all inflammation is your enemy. When you sprain your ankle or get a splinter, the swelling and heat actually help you heal faster.
This protective response increases blood flow to bring healing nutrients and immune cells exactly where they're needed. The inflammatory signals coordinate a complex cleanup and repair process, while the pain keeps you from causing more damage to the injured area.
The key difference is timing. Healthy acute inflammation turns on when needed and turns off when the job is done. It's this natural on-off switch that gets stuck in chronic inflammatory conditions - and it's exactly what acupuncture for inflammation helps restore.
Acupuncture 101 – From Ancient Meridians to Modern Clinics
Thousands of years ago, Chinese healers mapped an invisible network of energy pathways running through the human body. They called these pathways meridians and believed that life energy, or Qi (pronounced "chee"), flowed through them like rivers carrying vital force to every organ and tissue.
Along these meridians, they identified over 2,000 specific points where thin needles could influence this energy flow. To modern ears, this might sound like ancient mysticism. But here's where it gets interesting: 70% of neurogenic (hypersensitive) spots coincide with traditional acupuncture point locations.
These points aren't just theoretical. They actually show higher electrical conductance than the surrounding tissue. In other words, there's real, measurable anatomy behind those ancient maps.
When it comes to acupuncture for inflammation, one point stands out as a superstar: ST36 (Zusanli). Located on your lower leg, about four finger-widths below your kneecap, this point has been studied extensively by researchers. Time and again, studies show that stimulating ST36 produces powerful anti-inflammatory effects throughout the body.
Electroacupuncture takes this ancient practice into the modern age. By passing mild electrical current between needles, practitioners can amplify the treatment's effects. The results can be dramatic - in animal studies, mice treated with preventive electroacupuncture before a cytokine storm saw their survival rates jump from 20% to almost 80%.
The World Health Organization has taken notice, officially recognizing acupuncture's effectiveness for 16 inflammatory diseases. Today, you'll find acupuncture integrated into hospitals, pain clinics, and wellness centers across the country.
Tools & Techniques
Modern acupuncture practitioners have several tools in their toolkit. Traditional needling uses hair-thin, sterile needles inserted at specific depths - much thinner than the needles used for injections. Electroacupuncture adds gentle electrical stimulation to boost the treatment's power.
Some practitioners use moxibustion, burning dried mugwort herb to create therapeutic heat at acupoints. For those who prefer needle-free options, laser acupuncture applies light therapy to the same points. Cupping therapy, which creates suction on the skin, is often combined with needling for improved effects.
What a Typical Session Looks Like
Walking into an acupuncture clinic for the first time can feel a bit mysterious, but the process is straightforward. Your practitioner will start with a thorough assessment, asking about your symptoms, medical history, and specific inflammatory patterns.
Next comes point selection. Based on your condition, they'll choose specific points that research shows are most effective for your type of inflammation. The needle insertion happens quickly - most people are surprised by how little they feel.
You'll then rest comfortably for 20-30 minutes with the needles in place. During this time, you might notice interesting sensations - tingling, warmth, or a dull ache. These are all normal responses and often indicate the treatment is working.
Safety protocols are strict in professional settings. Licensed practitioners follow rigorous standards for needle sterilization and disposal. When choosing a practitioner, make sure they're properly licensed and follow established safety guidelines. More information about professional acupuncture services can help you understand what to look for in a qualified provider.
How Acupuncture Lowers the Inflammatory Flame – The Science
Tiny needles create big changes because they tap into the vagus nerve, a communication superhighway linking brain and body. When a point such as ST36 on the leg is stimulated, signals travel up the vagus, telling the adrenal glands to release dopamine. Dopamine then cools inflammatory cytokines like TNF-α and IL-6 in tissues from joints to gut.
Researchers confirmed this by removing adrenal glands in mice: without dopamine, the anti-inflammatory effect disappeared. Give those same mice a dopamine-boosting drug and inflammation still dropped, proving the pathway’s importance.
Acupuncture also steadies the HPA (hypothalamic-pituitary-adrenal) axis and rebalances the sympathetic “fight-or-flight” response. The result is a coordinated switch from pro-inflammatory to healing signals:
Lower IL-6, TNF-α, IL-1β
Higher IL-10 (your body’s own anti-inflammatory messenger)
Activation of the antioxidant Nrf2/HO-1 system
Shifts macrophages from destructive M1 to reparative M2 states
At the genetic level, needling quiets microRNA-155, a master on-switch for many inflammatory genes, and engages CB2 receptors of the endocannabinoid system for natural pain control. Scientific research on these pathways shows the changes are measurable and repeatable.
What Animal Studies Tell Us
• Sepsis models: electroacupuncture at ST36 boosted survival from 20% to nearly 80%.
• Colitis mice: reduced gut inflammation and improved barrier function.
• Arthritis rodents: immune cells flipped from M1 to M2, limiting joint damage.
These findings help explain why many people feel steadier, less swollen, and more mobile after a short series of treatments.
Acupuncture for Inflammation: Evidence Across Conditions
A 2021 review of 363 basic studies concluded that acupuncture lowers inflammatory activity in the immune, digestive, respiratory, nervous and vascular systems. Roughly half of patients report 50 % or better pain relief, a result comparable to NSAIDs but with far fewer risks.
Treatment Aspect Acupuncture NSAIDs Efficacy 50 % reach ≥50 % pain reduction 60-70 % for acute pain Onset 2-6 sessions Hours to days Side Effects Mild bruising, temporary soreness GI bleeding, kidney strain Gut Impact May strengthen gut barrier Often irritates gut lining Long-term Use Generally safe Higher cardiovascular risk
Joint Pain & Arthritis
Across 43 studies on rheumatoid arthritis, acupuncture improved function, cut morning stiffness, and lowered lab markers such as ESR and C-reactive protein. Osteoarthritis data are mixed but many hip and knee patients still report noticeable day-to-day relief, especially when electroacupuncture is paired with exercise.
Gut on Fire: IBD
Small trials in Crohn’s and ulcerative colitis show fewer flares, less abdominal pain, and stronger intestinal barrier proteins after 8–12 sessions. The vagus-gut connection appears central to these benefits.
Breathing Easier: Asthma & COPD
Needling calms airway inflammation, reduces bronchial reactivity, and nudges the immune system away from Th2 dominance. Many clients end up using rescue inhalers less often.
Skin, Nerves and Beyond
Eczema itching, neuropathic burning, migraine frequency, and even treatment-related cancer pain have all improved in controlled studies. The common thread is reduced neuro-inflammation.
Practical Guide to Using Acupuncture in an Anti-Inflammatory Plan
First, pick a licensed acupuncturist with at least four years of formal training and experience treating inflammatory conditions. Sterile, single-use needles and clean technique are non-negotiable.
Sessions in Oklahoma City or our nearby locations (Yukon, Edmond, Nichols Hills, Del City, Mustang, Moore) typically cost $75-$200. Many insurance plans now offset a portion of that fee, so check your benefits.
Most clients start with 2-3 visits a week for two to three weeks, then taper to weekly or bi-weekly maintenance. Early changes often appear by the third or fourth visit.
Choosing Points and Techniques
• ST36 (Zusanli) for whole-body inflammation.
• Local points near painful joints or organs for targeted relief.
• Low-frequency electroacupuncture (2-10 Hz) works well for stubborn chronic inflammation.
Working With Your Medical Team
Acupuncture pairs safely with NSAIDs, steroids, or biologics, but always tell your prescribing physician when you begin treatment. The combined approach often lets you lower medication doses over time.
Situations Requiring Caution
Bleeding disorders, certain blood thinners, pregnancy (some points are off-limits), active skin infections, or unstable heart conditions need special handling. A qualified practitioner will screen for these during intake.
With the right plan, acupuncture becomes a practical, low-risk way to quiet inflammation while supporting the spine-focused work we do every day at ChiroHer.
Frequently Asked Questions about Acupuncture for Inflammation
Does acupuncture work immediately for inflammation?
Here's the honest answer: acupuncture for inflammation isn't like taking an aspirin. While some patients feel a sense of relaxation or mild relief right after their first session, the real anti-inflammatory magic happens behind the scenes over several days.
Remember how we talked about acupuncture activating your vagus nerve and triggering dopamine release? That process takes time to build momentum. Your immune system needs to shift from producing inflammatory chemicals like TNF-α and IL-6 to creating more anti-inflammatory messengers like IL-10.
Some lucky patients notice their joint stiffness easing or their pain decreasing within 24-48 hours of treatment. But for most people, it's more like watching a garden grow - the changes are gradual but meaningful.
How many sessions before I notice reduced swelling or pain?
Most of my patients start seeing real improvements somewhere between their second and sixth sessions. That usually translates to about 2-4 weeks of consistent treatment, assuming you're coming in 2-3 times per week initially.
Here's what typically happens: Week 1 might feel like not much is changing. Week 2 is when people often say "I think something's different, but I'm not sure." By Week 3-4, the improvements become more obvious - less morning stiffness, better sleep, or that nagging pain finally backing off.
Chronic inflammatory conditions like rheumatoid arthritis or inflammatory bowel disease often need more patience. Some patients require 8-12 sessions before seeing significant changes. Think of it this way: if your inflammation took months or years to develop, it's reasonable to give your body a few months to heal.
The key is sticking with your treatment plan. Sporadic sessions won't give you the cumulative benefits that make acupuncture for inflammation so effective.
Can I replace my anti-inflammatory meds with acupuncture?
This is probably the most important question, and I need to be crystal clear: never stop prescribed medications without talking to your doctor first. I've seen patients get into trouble by making medication changes on their own, even with the best intentions.
That said, acupuncture often works beautifully alongside conventional treatments. Many patients find they can gradually reduce their NSAID doses or use them less frequently as their acupuncture treatments progress. Some even work with their doctors to space out steroid injections or reduce other medications.
The smart approach is creating a team between you, your physician, and your acupuncturist. Your doctor understands your medical history and medication interactions. Your acupuncturist knows how to maximize the anti-inflammatory benefits of needle therapy. Together, they can create a safe plan that might allow you to use fewer medications over time.
At ChiroHer, we always coordinate with our patients' other healthcare providers. We want you to get the best of both worlds - the powerful anti-inflammatory effects of acupuncture combined with the safety net of medical supervision when needed.
Key Takeaways
Acupuncture for inflammation represents something truly remarkable - a bridge between ancient healing wisdom and cutting-edge scientific understanding. When you look at the research, it's clear that those thin needles can actually rewire how your immune system responds to inflammation.
The science is particularly strong for chronic pain conditions like arthritis, where inflammation becomes a stubborn, ongoing problem. We're also seeing compelling evidence for inflammatory bowel diseases, respiratory inflammation, and those tricky stress-related inflammatory conditions that seem to affect everything at once.
What I find most exciting is how acupuncture works with your body's natural systems. Instead of blocking inflammation like medications do, it teaches your vagus nerve and immune system to communicate better. It's like giving your body's internal healing team better coordination skills.
At ChiroHer, we see inflammation from a whole-body perspective. When someone comes in with back pain, we're not just looking at their spine - we're considering how inflammation might be affecting their entire system. Sometimes the missing piece isn't another spinal adjustment, but helping calm that underlying inflammatory fire.
Our patient-focused approach means we take time to understand your complete health picture. While we specialize in chiropractic care, we absolutely recognize when acupuncture might be exactly what your body needs to break the inflammation cycle.
The key is finding practitioners who understand both the traditional art and the modern science. You want someone who can explain exactly how they're targeting your specific inflammatory condition, not just placing needles randomly and hoping for the best.
Inflammation is actually your body trying to heal itself - it just sometimes needs a little guidance to do it more efficiently. Whether through personalized chiropractic care, acupuncture, or other natural approaches, the goal is always supporting your body's amazing ability to heal.
Ready to explore how acupuncture might fit into your anti-inflammatory plan? Start by having an honest conversation with your healthcare providers about what you're experiencing. Research qualified practitioners in your area, and don't be afraid to ask questions about their experience with inflammatory conditions.
Your path to better inflammatory balance might be simpler than you think - and it definitely doesn't have to involve a lifetime of medication side effects.